What is a colonoscopy? When is it done?

What is Colonoscopy?
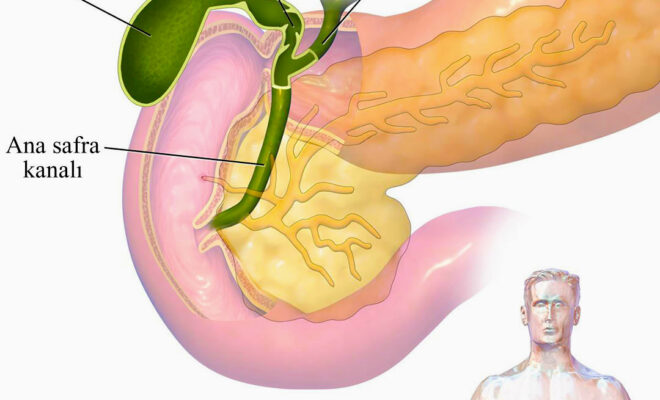
It is the procedure in which the rectum, large intestine and the last part of the small intestine are examined. This procedure is performed with a colonoscope, which is a flexible and thin cable-shaped instrument. The doctor performs the examination with the image transmitted to the monitor from the camera at the tip of the device. Thanks to the special channels in the colonoscope, washing, aspiration and, if necessary, interventions can be performed with special equipment.
When is a colonoscopy performed?
- Problems with defecation
- Change in defecation habits
- Persistent abdominal pain
- rectal bleeding
- Chronic Constipation
- chronic diarrhea
- Unexplained iron deficiency and anemia
- Unexplained weight loss
- Positive fecal occult blood test
- Starting from the age of 50, every person should be screened for colon cancer every 5 years.
- In patients with a family history of colon cancer at an early age, colon cancer screening should be performed at an earlier age.
What kind of preparation is required for the procedure?
At least 8 hours of fasting is required for the colonoscopy procedure. If it is to be performed under anesthesia, all liquid foods, including water, must be stopped at least 2 hours beforehand. Preparations (such as consuming liquid foods and using bowel cleansing drugs) must be made 24 hours before the procedure in order to prevent the solid stool in the colon from obstructing the camera examination during the procedure.
Patients who use blood thinners, have bleeding-related diseases, and rheumatic heart valve disease should inform their doctor about these conditions during the pre-procedure interview in order to avoid making the procedure risky.
How is the Colonoscopy Procedure Done?
Patients who want the procedure to be performed under anesthesia are given intravenous sedation and the procedure begins after the patient becomes asleep. Since the procedure is not a surgical intervention, general anesthesia is not required.
The endoscopy device is entered through the anus and the rectum, large intestine and, if necessary, the last part of the small intestine are examined. The procedure is technically more difficult than gastroscopy and takes an average of 12-15 minutes. This period may be extended in cases requiring biopsy and intervention.
The biopsy process is performed by removing millimetric-sized pieces from suspicious areas with small equipment. This procedure does not cause bleeding or post-procedure pain. The samples taken are sent to the pathology laboratory for microscopic examination.
In cases where the lesion must be completely removed (for example, polyp removal) or bleeding must be stopped, procedures are performed with different apparatus.
What is it like after the procedure?
If the procedure was performed with sedative anesthetics, you will be discharged after being kept under observation for 30-45 minutes. 3-4 hours of rest at home is recommended. In addition, with plenty of movement, gas is released and the feeling of bloating after the procedure is reduced. Liquid foods can be consumed after 2 hours. After 6-8 hours, solid foods can be started. After procedures performed under sedation, patients should not do tasks that require attention, such as driving, on the same day. If the procedure will be performed under sedation, you must come to the procedure with a relative who will drive you home.
Is there any risk?
Since the procedure is usually performed under sedation, there is no pain. However, since the inner surface of the intestine is examined by inflating it with gas, swelling occurs after the procedure. The procedure should never be performed on a full stomach. Otherwise, stomach contents may escape into the lower airways during the procedure and cause conditions such as infection and suffocation.
Sterilization of the instruments to be used in the procedure is very important to protect against infections. In inexperienced hands, there may be risks such as bleeding and perforation. Therefore, be careful when choosing the place and doctor where you will have the procedure done.
In what situations should you call your doctor after discharge?
- Abdominal pain that does not get better and gets worse
- Increasing abdominal bloating
- Persistent nausea and vomiting
- bloody defecation
- Fire
Op. Dr. Cemal Seyhun
General surgery specialist
Contact Us For Appointment:
Telephone line: 0392 444 3548 (ELIT)
Contact Form: https://www.elitenicosia.com/iletisim/