Idiopathic Scoliosis in Children and Adolescents

Scoliosis is a condition that causes the spine to curve sideways. There are several different types of scoliosis that affect children and adolescents. The most common type of scoliosis is the "idiopathic" type, whose cause is unknown.
Most cases of idiopathic scoliosis occur between the age of 10 and when the child is fully grown. Scoliosis is rarely painful. Small curves often go unnoticed by children and their parents and are first detected during a school screening or at a regular check-up with the pediatrician.
In most cases, scoliosis curves are minor and do not require treatment. Children with larger curves may need to wear a splint or have surgery to restore normal posture.
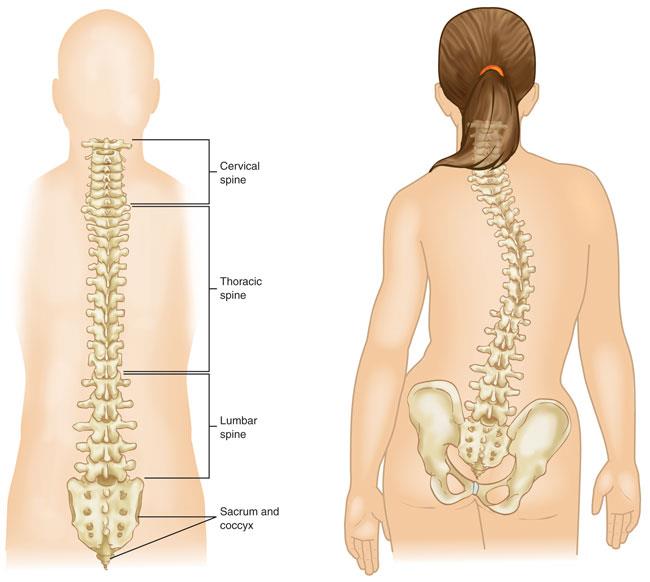
(Left) Normal spine anatomy. (Right) Scoliosis can cause the spine to look more like the letters “C” or “S.”
Definition:
Scoliosis causes the bones of the spine to bend or rotate. Thus, the straight line in the middle of the back resembles the letter “C” or “S”. Although scoliosis curves most commonly occur in the upper and middle back (thoracic spine), they can also develop in the lower back. Sometimes they can even occur in both the upper and lower parts of the spine.
Idiopathic scoliosis curves vary in size. Mild curves are more common than larger curves. If the child is still growing, the scoliosis curve may worsen rapidly during a growth spurt.
Although it can develop in young children, idiopathic scoliosis most often begins in adolescence. While both boys and girls can be affected, girls are more likely to develop larger curves that require medical care.
Other less common types of scoliosis include:
Congenital scoliosis: Problems in the spine develop before the baby is born. Babies with congenital scoliosis may have spinal bones that are not fully formed or fused.
Neuromuscular scoliosis: Medical conditions that affect the nerves and muscles, such as muscle diseases or cerebral palsy, can cause scoliosis. Such neuromuscular conditions can cause instability and weakness in the muscles that support the spine.
From where:
Although the exact cause of idiopathic scoliosis is unknown, it is known that it is not related to certain behaviors or activities (such as carrying a heavy backpack or poor posture).
Araştırmalar bazı durumlarda genetiğin skolyoz gelişiminde rol oynadığını gösteriyor. Ergen tipi idiyopatik skolyozu olan hastaların yaklaşık %30’unda bu duruma ilişkin bir aile öyküsü vardır.
Symptoms:
Minor curves often go unnoticed until the child reaches a growth spurt during adolescence.
Examples of symptoms:
One shoulder blade may protrude more than the other
There may be a level difference between shoulders
The prominence of the ribs may increase on one side
irregular waist
One hip may sit higher than the other
Many cases of scoliosis are first detected during a school screening or regular pediatric exam.
If your pediatrician suspects scoliosis, he or she may refer you to a pediatric orthopedic surgeon or spinal deformity surgeon for a complete evaluation and treatment plan.
Medical examination
Physical examination:
The standard screening test for scoliosis is the “Adam's forward bend test.” During the test, your child will lean forward with his feet together, knees straight, and arms free. Your doctor will observe your child from behind, looking for a difference in the shape of the ribs on each side. Spinal deformity is most noticeable in this position.
While your child is standing upright, your doctor will also check whether his hips and shoulders are straight and whether the position of his head is above the hips. It will control the movement of the spine in all directions.
To rule out other causes of spinal deformity, your doctor will check for limb length discrepancies, abnormal nerve findings, and other physical problems.
X-ray:
X-rays will provide clear images of the bones in your child's spine. They allow your doctor to see the exact location of the curve and measure how severe it is. In general, curves greater than 25 degrees are considered serious enough to require treatment, depending on the age of the child.
Treatment
Your doctor will consider several things when planning your child's treatment:
Location of curvature
Severity of curvature
Your child's age
Number of remaining growing years (rapid worsening of the curvature is not common once the adolescent is fully grown).
By evaluating these factors, your doctor will determine how much your child's curve will worsen and can recommend the best treatment option.
Non-Surgical Treatment:
Observation: If your child's spinal curvature is less than 25 degrees or is almost fully grown, your doctor may recommend monitoring the curvature to make sure it doesn't get worse. Your doctor will recheck your child approximately every 6 to 12 months and take follow-up X-rays until your child is fully grown.
Brace: If the spinal curvature is between 25 and 45 degrees and your child is still growing, your doctor may recommend a brace. Although bracing does not correct an existing curve, it usually prevents it from getting bad enough to require surgery.
A recent study of scoliosis patients with curves at high risk of worsening showed that bracing treatment significantly reduced the incidence of curves progressing to the point of requiring surgery.
Surgical treatment:
Spinal Fusion:
If your child's curve is greater than 45 to 50 degrees or if the brace did not prevent the curvature from reaching that point, your doctor may recommend surgery. Severe curvatures that are left untreated can eventually worsen to the point of affecting lung function.
A surgical procedure called spinal fusion will significantly correct the curvature and then fuse the vertebrae together into a single solid bone. This will completely stop growth in the part of the spine affected by scoliosis.
During the procedure, the spinal bones that create the curvature are realigned. Small pieces of bone called bone grafts are placed in the spaces between the vertebrae to be fused.
Metal rods are typically used to hold bones in place until fusion occurs. The rods are attached to the spine with hooks, screws and/or wires.
Exactly how much of the spine needs to be fused depends on your child's curve(s). Only the curved vertebrae are fused together. Other bones of the spine continue to move and assist in movement.
Rehabilitation:
On the first day after spinal fusion surgery, most patients can walk without wearing a brace. Discharge from the hospital is usually 3 to 4 days after surgery. Most children can return to school and resume daily activities within 4 weeks.
Long Term Result:
Spinal fusion is very successful in stopping the curve from growing. Surgery can also significantly correct the curve, improving the patient's appearance.
Most children can return to sports activities 6 to 9 months after surgery. Because the surgery causes some spinal movements to be permanently restricted, participation in contact sports such as football may be discontinued.
Spinal fusion does not increase girls' risk of complications during future pregnancies or births.
Op. Dr. Barış PEKER
orthopedics and Traumatology specialist
Contact Us For Appointment:
Telephone line: 0392 444 3548 (ELIT)
Contact Form: https://www.elitenicosia.com/iletisim/